Procedural Pearls, in the RAW.
This month, instead of a focused procedure, we want to answer:
“What ER and urgent care procedures do I REALLY need to know as an APP?”
Here we go, a “raw blog” as many of your have requested!
This may be a little controversial, but I feel like procedures are one of the places where we can really demonstrate our value as PAs and NPs. Things can grind to a halt in an ED or an urgent care clinic when a procedure comes in and a clinician is required to be at bedside for an extended period of time. With the workflow of most EDs, it might be preferable that a PA or an NP be the one to do the procedure.
Everyone, students and even seasoned professionals are always asking me, “what are you good at” and “how did you learn that” and “how did you do that” and “what should I be best at? I say one thing to them: “Don’t get too comfortable”. When you get comfortable, that’s when you forget things and make mistakes, so I like to keep it fresh, watch others on their technique and modify mine by being open minded and always working on going from being good to great. No one is perfect and we must all keep the basics in mind, don’t get too fancy. Sure. There are some fancy things - but don’t get too confident. Be sure to know these procedures well before doing things like joint injections, occipital blocks and nerve blocks. Vessel loop for abscess has promise and can be great for patients - but simple I/D is really the treatment. Nasal intubation - great skill - but do 100 regular intubations before even contemplating this one. And that is just a few of the thousands of procedures we can do.
Learn. Repeat. Watch. Practice before implementing, see one do one teach one.
Be decent at THESE things and be that fire in someone’s pocket when the storm is breaking out in your department.
You want people to know you for your work, just like an artist.
And, before I go into them, I want to say that The Procedural Pause for Emergency Medicine News covered every single one in detail over the last 10 years and you can access the videos and the blogs to update yourself – just click on the link above to the homepage. Be sure to check out the archives! And if you want the best procedural book out there, might I suggest Roberts & Hedges - but I am a bit biased on that one. 8th edition coming to an ED near your soon!
Here are some suggested top 10 procedures to focus on this year:
(we also cover them all on The Procedural Pause)
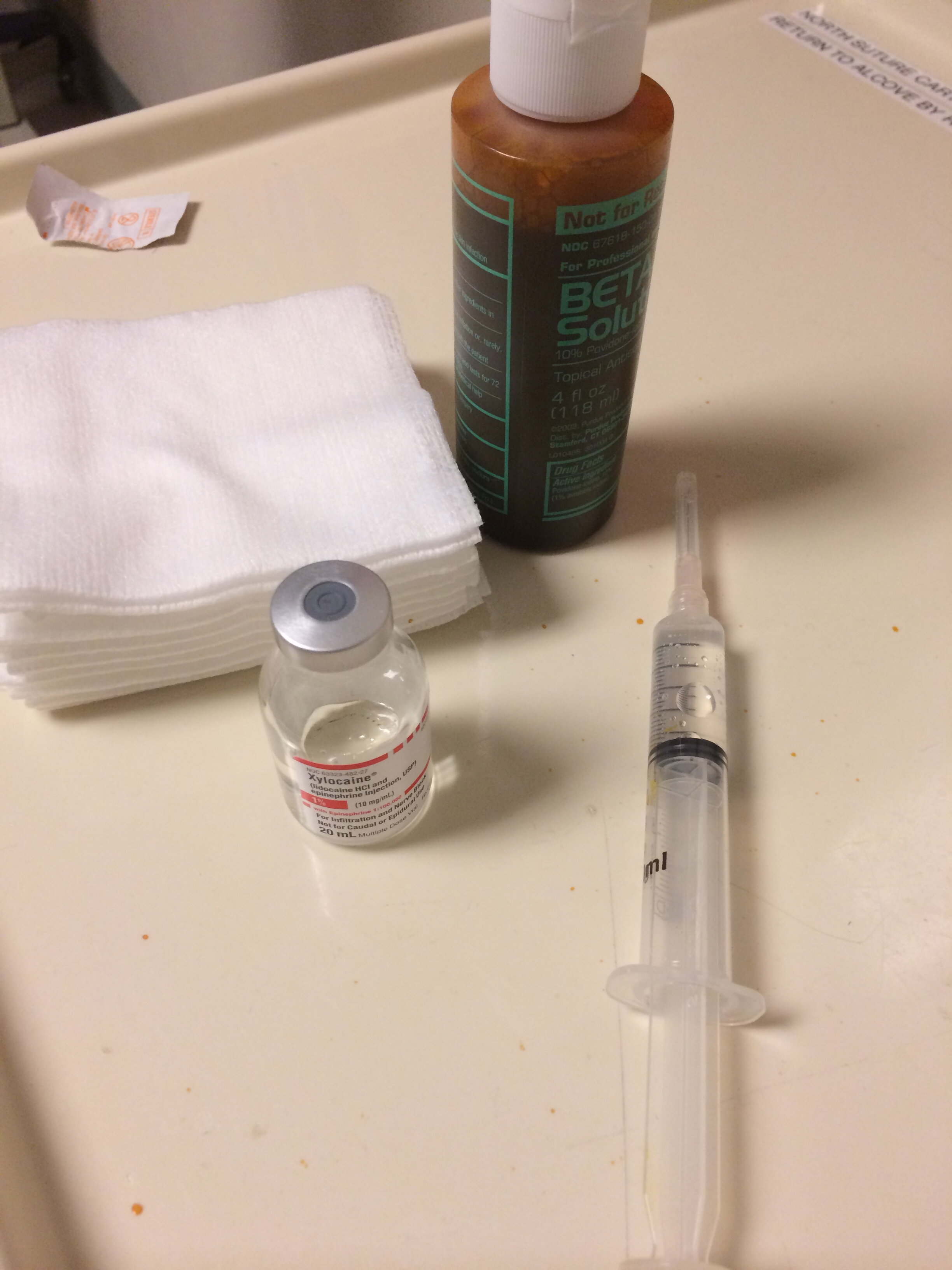
1. Suturing and laceration repair, generalized wound care
2. Abscess treatment and the essentials for incision and drainage
3. Reductions
4. Splinting (of course comes next)
5. US guided IV access or SOLID IV access skills!
6. Ear wax removal – and other ENT procedures
7. Any ocular procedure and slit lamp exam to find it
8. Nasal packing and how to stop the bleeding
9. NG tube placement
10. LPs OR central line (which I’ll get to shortly why it’s ok to choose for a short time) and then master both!
Yes, this is going to sort of be a food for thought list and motivational discussion for all those reading. First of all, this top ten (minus intubation) are the top procedures done in the ER. Yes, emergent procedures in the ER. ENT procedures are high up there on the APP skill list as well as lines and drains - I like to add a bonus that being able to know your way around ANY tube and drain is a must such as placing foleys, cuades, jp drains and reinserting feeding tubes. KNOW ALL THE TUBES AND DRAINS. Check out our other newish blogs up on skin grafts and drains HERE on this site! You can start by taking a look at for a quick review of JP drains this month.
I want to say that knowing how to suture and do a proper ID is crucial in fast track. Identify, do the procedure efficiently and quickly, painlessly. And, knowing when to call plastics for something you can’t handle and knowing when to call general surgery if the abscess is concerning for “more” or admission etc. And, knowing whether you need to transfer patients based on your assessment. Get really good at knowing what you can, can’t do and should do for patients, which is your first lesson before cutting anything. There are lots of suturing techniques, but my main focus here is knowing the simple interrupted and the mattress - those are key. Master these! Your technique is super important and the time in which you can do good work
I tend to avoid the running suture unless within a tight space like toes and finger webs, armpits, underwear line etc - where you don’t want poking knots. I’m not a fan for the scarring they may cause - and they can get sloppy. But I appreciate the quick fix in areas well-hidden or as I mentioned, don’t need a bunch of knots poking around.
The other thing I want to talk about is splinting and reductions. You need to be the GO TO PERSON in your ER for splinting. Don’t call ortho or the tech to do it. You do it. That is also why reductions are on the list because if you know what you’re dealing with and you reduce it - only you know how to put on the right splint - so do it and do it correctly.
And US guided IVs. Now, those superficial veins are not great and sometimes you have to go deep. Despite your awesome blind technique, the vein is going to blow. The patient doesn’t need15 sticks. The key here is take the course at your hospital (usually offered by the nursing team) on how to put in an US guided IV. Once you learn how to do this, you will get all excited about US and want to do way more, that’s when you can come to our bootcamp courses and then find a mentor on your site to help you get credentialed to do specific procedures like US guided nerve blocks, paracentesis, ocular exams, DVT etc.
But what about ear wax? And other ENT procedures? The answer to this involves two answers - ear wax removal is an easy skill that you need to do. The first answer is that it’s an easy procedure to fix (just add drops, wait and irrigate) and 2. Patients perhaps will get immediate relief. You’re right, you’re thinking to yourself, it’s not emergent. But, it makes people feel better – your main goal on the job! This is a super easy procedure to do. It gives a patient relief. Not fixing it is not going to stop the patients from coming in. Sure, it’s not an emergency but hey, this patient is here and you can fix it so why not. And, who knows, maybe the patient has an infection brewing back there and now you’ve cleared the road to help them heal. Remove ear wax. It’s ok to do it in the ER or urgent care and it’s an important skill.
This brings me to more head and neck issues in the ER. I want to slip in these two thoughts - knowing how to do a good ocular exam and diagnosing ocular issues is so critical for APPs. Not only are there a million diagnoses with eye pain, trauma, vision loss and blurry vision - but treating traumatic eye injuries seems to be a top procedural skill APPs do in the ER. Again, I work with physicians who will pick up the patient and ask me to do the slit lamp exam and eval. I feel great doing this - because I am GOOD at the exam. It only takes about 15 minutes to learn how to do a STELLAR exam and it is crucial.
Here is my quick thought on NG tubes. The reason why this one makes this list is because this is hard to do sometimes. Awake patients- tough. You have the have “the touch” and there are a lot of pearls you need to keep in mind when inserting one. Tough stuff and patients need you to hold their hand, literally. It’s not just about being able to get the tube down, it’s about comforting the patient. Think about if you had to get a tube shoved down your nose.
And my final pearl: I have found that some of the APPs in my department are great at LPs and others are great at central lines. I really like owning one of these procedures. I know physicians whom I work with who will ask me to attempt if they miss. That feels like an honor for me - and sometimes it just takes a different eye and steady hand. As for the central line, again - during an intubation or trauma, everyone needs a job. If you can pop in a central line while the physician is intubating - think about how much time is saved and patients will get better care. Now, I’m not saying you can only be good at LPs or central lines, but those two big procedures both need a lot of practice and I am hoping that you too can be a “go to” person in your department for this skill if needed.
So those were just some procedural pearls of wisdom I really wanted to share with you guys this month. Remember - don’t get comfortable. Keep it classy and current and always watch others!! Check out all techniques. It will only take you from good to great.
The Proceduralist YouTube site (browse 100s of procedural videos, as mentioned on the podcast): https://www.youtube.com/c/ProceduralPausetheproceduralist/videos - Hopefully something tickles your fancy.
Here are a few links we mentioned in The 2 View podcast, episode 5.
Procedure: Slit Lamp Exam
Procedure: Cerumen Impaction
Procedures: Ear Wicks
Procedure: Ankle relocations and splinting
Procedure: Some lower leg splinting
Procedure: Tonometry
Procedure: TXA / Epistaxis
Procedure: Lumbar Puncture (Part I in a series)
Procedure: Central Line Tie Down
As always, we got you.
Send questions and feedback to 2viewcast@gmail.com